Abstract

Background and Objectives: Hypertension is an established risk factor for subsequent cardiovascular and renal disease in children as well as adults. Sickle Cell Disease (SCD) is a genetic disorder associated with anemia with the major manifestation of vaso-occlusive crises. While this disease entity involves most organ systems causing vascular and pulmonary injury, little is known about blood pressure (BP) levels or prevalence of hypertension in children and adolescents with SCD.
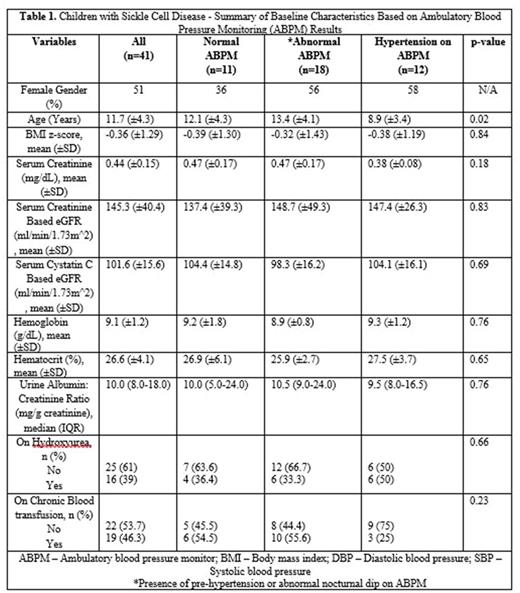
Methods: We enrolled 41 children with severe genotypes of SCD (39 with Hb SS disease and 2 with Hb Sβ0 thalassemia). Study participants underwent 24-hour ambulatory blood pressure monitoring (ABPM). Clinical information regarding duration of SCD, SCD-related complications, requirement for chronic blood transfusion and chronic hydroxyurea therapy were obtained. Baseline characteristics obtained on each participant included age, gender, weight, height, body mass index (BMI) percentile, BMI-Z score and clinic BP. Serum creatinine and cystatin C were obtained to assess estimated glomerular filtration rate (eGFR) with age-based formulas. A random urine sample was obtained for standard urinalysis, albumin and creatinine estimation, to calculate urine albumin to creatinine ratio.
Results: Based on ABPM study results participants were categorized into three groups as normal ABPM, abnormal ABPM, or hypertension ABPM (ambulatory hypertension, masked hypertension or severe ambulatory hypertension). The term abnormal ABPM designated participants who did not have normal ABPM or hypertension, but had other abnormal parameters on ABPM (presence of pre-hypertension and/or lack of normal nocturnal dipping). SCD children in the three groups were similar with respect to distribution of age, BMI z-scores, renal function, urine albumin excretion, urine osmolality, hemoglobin, history of chronic blood transfusion, and hydroxyurea therapy. Twelve participants (29.3%) met criteria for hypertension based on ABPM. Of the 12 hypertensive participants, three had clinic hypertension with ambulatory hypertension; and nine had masked hypertension detected on ABPM. Youngest child with ABPM confirmed hypertension was six years of age. Another 18 participants (43.9%) had some abnormal ABPM parameters that were largely present in the sleep period of ABPM.
Conclusions: Findings from our study indicate that BP abnormalities are not uncommon in SCD children. Overall, the distribution of confirmed hypertension, largely manifested by masked hypertension, is high in pediatric participants with SCD; as young as 6 years of age. The underlying cause for the relatively high prevalence of masked hypertension and abnormal ABPM parameters including absence of nocturnal BP dip in children with SCD is unclear. Based on our findings more attention should be given to monitoring and management of BP in children with SCD. Early identification of hypertension in SCD children can confer benefit because hypertension is an important modifiable risk factor for progression of cardiovascular and renal disease.
Acknowledgment: Research reported in this publication was supported by the National Institute Of General Medical Sciences of the National Institutes of Health under Award Number P20GM109021; National Kidney Foundation Young Investigator Grant and DE-CTR-ACCEL grant number U54-GM104941 (PI: Binder-Macleod).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal